Pediatric cardiopulmonary arrest occurred in all ages of children. The common accidents causing cardiopulmonary arrests in adolescents are traffic accidents, drowning and burns, while breath holding is usually the initiating event of arrest in premature babies. Pediatric Basic Life Support ( PBLS ) emphasizes the importance of keeping airway patent; providing optimal mouth- to-mouth breathing, and undergoing incessant cardiac massages.
Procedure of PBLS
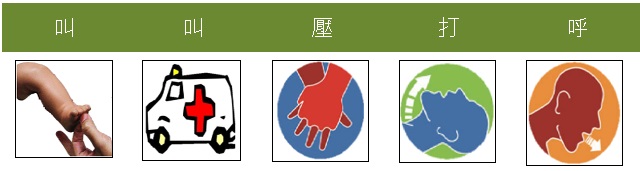
- Check consciousness and response: When there is lips cyanosis, upward gazing, or consciousness disturbance, the rescuer should assesses patient’s response by shoulder-tapping, feet-rubbing as well as shouting at his/her face. If there is no response, call for help ( or phone 119 ) and start one-man cardiopulmonary resuscitation ( CPR ) immediately.
- Position the victim : Position the victim in a supine posture on a flat, hard surface, such as floor or ground. If you must turn the victim over, you should avoid turning or twisting the victim’s neck but support his/her head-and-neck axis with a firm forearm lain behind the patient’s neck.
- Confirm site safety: First determine the safety of the rescue environment to avoid disaster expansion. And pay attention to clues at the scene, such as unusual smells or temperatures, empty medicine bags or cans, exposed wires, etc.
- Open the airway:
- Remove any foreign substance inside the mouth
- When there is no evidence of trauma, open his/her airway with a ‘head tilt-&-chin lift’ maneuver.
- If a cervical spine injury is suspected, use ‘ jaw thrust ’ maneuver rather than ‘head tilt’ maneuver to open the airway
- maneuver rather than ‘head tilt’ maneuver to open the Check breathing:
- Observe breathing movement ( excursion of chest or abdominal wall ) and listen and feel for any air exhalation (get close to patient’s nose and mouth).
- If there is breathing, place the patient on the side (recovery position)
- If no breathing, give 2 blows of rescue breathings
- Use mouth-to-mouth breathing technique while pinching the victim’s nose tightly, or use mouth-to-mouth-and-nose technique on a small infant.
- Give every rescue breathing slowly and steadily for at least 1-1.5 seconds
- Make sure a concurrent chest wall rise occurs smoothly with each breath
- Check pulses
- Check brachial pulse on upper arm of infants and carotid pulse on neck in children
- If you cannot feel pulse in 10 seconds, proceed to chest compressions without delay
- Chest compressions:
- For infants < 1 year of age: push the sternum with the 2rd and the 3th finger on an area just below the intermammary line, Compress the lower sternum to a depth of 1.5 inches (4 cm) at least 100 - 120 times per minute.
- For children 1 to 8 years of age: compression on the lower half of the sternum but avoiding compression on the xiphoid process, compress the lower part of the sternum to a depth of 2.5 inches (5 cm), at least 100 - 120 times per minute.
- The following principles represent chest compression with good quality :
- “Push hard”: push sternum with sufficient force to depress the sternum to approximately one half depth of the anterior-posterior diameter of the chest.
- “Push fast”: push at a rate of approximately 100 compressions per minute.
- Release completely to allow a full chest recoil.
- Do not interrupt during chest compressions.
- Give every rescue breathing slowly and steadily for 1 seconds, Continue to do chest compressions and artificial respiration for 5 cycles (about 2 minutes).
- Coordinate chest compressions and breathings by a ratio of 30 : 2 (Thirty chest compressions followed by 2 effective breathings). Try to minimize interruptions when proceeding chest compression.
- Reassess patient’s consciousness, breathing and pulses every 2 minutes after CPR ( 5 cycles of compression-&-breathing ) : If spontaneous breathing and adequate heart beatings return, keep the victim in a recovery position; if not, continue CPR.


