Difficulties occur in the process of food entering the stomach from the mouth, leading to the inability to chew or swallow normally, which easily causes food or liquid to be inhaled into the trachea and further into the lungs by mistake. Long-term dysphagia can lead to malnutrition, dehydration, aspiration pneumonia, and other comorbidities.
Causes
Dysphagia is common in cerebral infarction, head injury, myasthenia gravis and other diseases.
Symptoms
- You cannot close your mouth and are drooling.
- Food is held in the mouth and cannot be swallowed or until several attempts.
- Food leaks out of your mouth when you are eating.
- Some food still remains in your mouth after eating.
- As soon as food is swallowed or eaten, you choke and cough. You may also cough and choke during eating.
- Eating takes extended time or multiple times.
Treatment
- For patients allowed to eat by the doctor, refer to “diet preparation” and “eating tips.”
- If adequate nutrition cannot be obtained via the mouth, nasogastric tube insertion or gastrostomy can be considered after the doctor's evaluation.
- When necessary, refer the patient to a speech therapist for swallowing training.
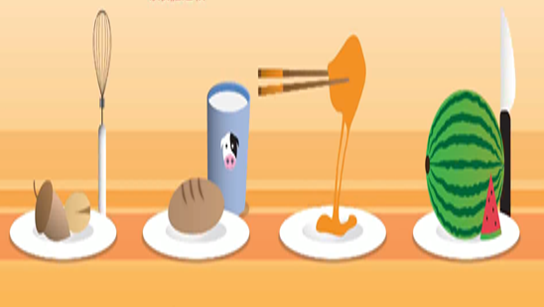
Diet preparation
- Water, milk, soymilk or other liquid foods should be thickened to different degrees according to the patient's swallowing ability. Thickeners can be used to increase the viscosity.
- Bread, steamed bread, cake, biscuits, hollow cake, etc. can be soaked with milk, soybean milk, fruit juice, etc. and then eaten with a spoon to avoid the bread being too dry to swallow or being choked by biscuit crumbs.
- Choose finely chopped or soft food as far as possible.
- Avoid food that is too sticky or bulky: such as glutinous rice products, tangyuan, rice cakes, sarong, pork balls, fish balls, etc.
- Harder fruits can be ground into paste with a grinder, such as apples, pears, and jujubes. Large fruits with seeds should be seeded before being sliced, to facilitate flesh chewing and avoid eating whole fruits directly, such as Annona squamosa, lychees, longans and grape.
Eating tips
- Sit upright at 90 degrees while eating.
- The food should be fed via the healthy side of the mouth. Avoid the use of a straw to prevent choking and coughing. Feeding should be done slowly with small spoons in small mouthfuls.
- Open your mouth when eating, put food in your mouth and chew it closed. Use your tongue to lift food up to the roof of your mouth and sallow it while tucking in your chin.
- Start with a small amount of about 30g. Eat in small bites. Each bite should be swallowed at least twice. Open your mouth after eating to check for complete swallowing before taking another bite.
- If you feel foreign body sensation in your throat but do not cough after swallowing, you can cough and clear your throat 1-2 times every 2-3 swallows.
- After eating, pay attention to clearing the food gathered on the left or right side of the mouth.
- Don't talk while eating. Focus on controlling the speed and eat slowly one mouthful at a time.
- Listen to your own voice after swallowing, and cough and clear your throat if the sound is muddy and watery.
- Stop eating immediately if choking and coughing occurs while eating, and eat after rest and relaxation. If coughing continues, stop eating and inform medical staff.
Follow-up treatment of dysphagia at home
- If dysphagia persists, the attending physician may evaluate whether to consult the rehabilitation department or the elderly preventive medicine department to perform swallowing rehabilitation.
- If the patient still suffers from poor appetite due to dysphagia two days later, the attending physician can evaluate during the follow-up visit whether to consult the gastroenterology department for gastrostomy to provide nutrition.

