News and Award
About CMUH
CMUH Smart ARDS Platform Helps Reverse the Critical Conditions of ARDS Patients
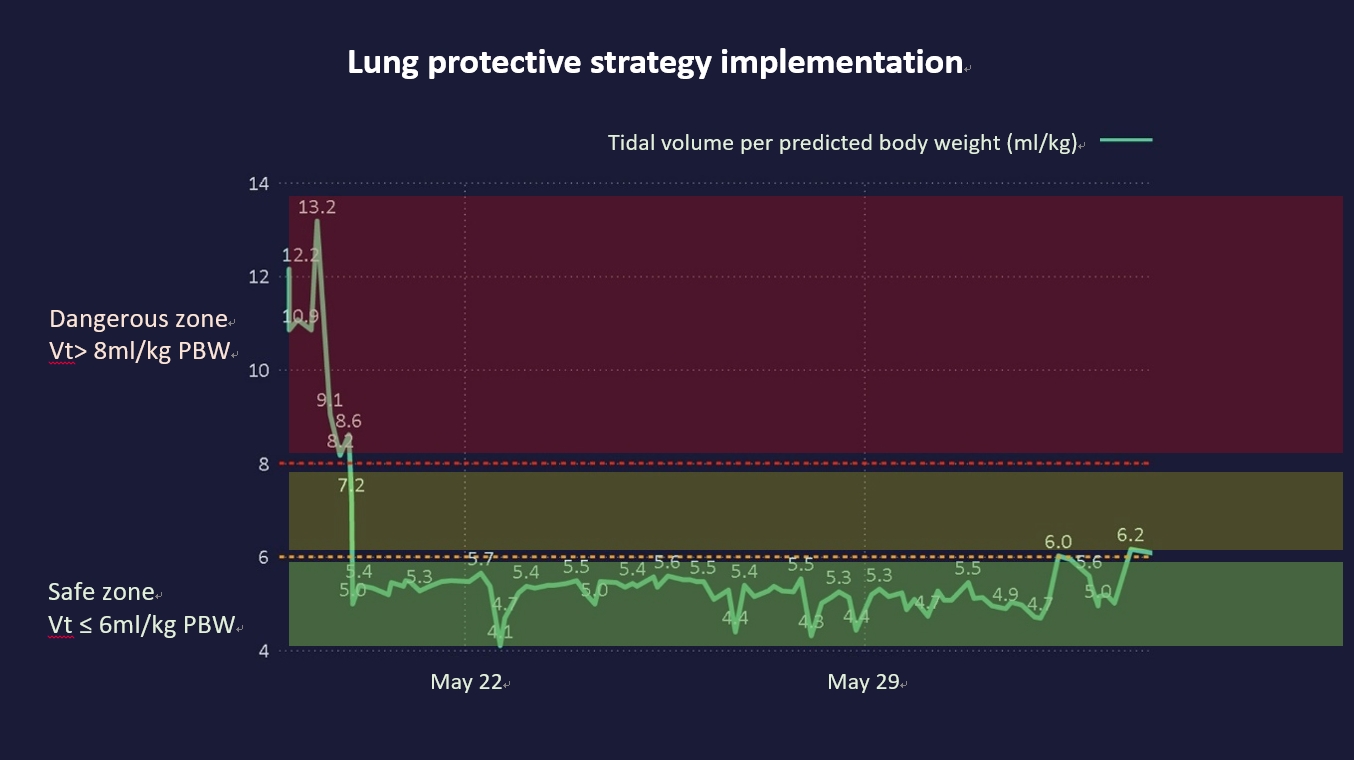
The 46-year-old of Ms. Chang, who had hypertension and nephropathy, accepted kidney transplantation surgery 10 years ago. On May 12th, 2022, Ms. Chang experienced repeated fevers and general weakness. She was tested positive for COVID-19, and her cycle threshold (CT) value was 17.5. Ms. Chang’s condition worsened quickly and her chest X-ray showed bilateral diffuse pulmonary infiltrations. Later, she presented shortness of breath with dramatically dropping concentration of oxygen saturation, so she clearly had severe respiratory failure and was diagnosed to have “Acute Respiratory Distress Syndrome (ARDS).” She could die at any minute. Ms. Chang immediately underwent endotracheal intubation and was transferred to the negative pressure isolation ICU at China Medical University Hospital. Once there, ECMO emergent use was initiated to temporarily replace the lung function of Ms. Chang. Furthermore, an interprofessional and cross-department ”ARDS team” was gathered right away to save Ms. Chang with all their combined efforts, including physicians from pulmonary and critical care medicine, renal transplantation, infectious diseases, and cardiovascular surgery, nurse specialists, the respiratory technicians team, technicians of extracorporeal technician, pharmacists, and nutritionists, who all teamed up to provide her with seamless care. The expert team applied the visualized smart medicine system to real-time monitor the key respiratory therapy “Lung Protective Ventilation (LPV)” for her and matching with the ECMO system in order to actively save Ms. Chang. Dr. Wei-Cheng Chen, V.S., Division of Pulmonary and Critical Care Medicine, said, according to her acute physiology and chronic health evaluation (APACHE) II score when she was admitted to the isolated ICU, the predicted mortality rate was 70%; however, the medical care team accurately provided the Tidal Volume (TV) to protect the lungs from injury through the assistance of the smart medicine system. They also gave the proper antibiotics and antivirals to the patient so that the condition of Ms. Chang was reversed and improved with 15 days of ECMO support. On the 23rd day, the endotracheal tube was removed, and Ms. Chang was getting stable and successfully recovered to be discharged after 35 days of hospitalization!
ARDS Needs Timely “LPV” Smart Medicine System Can Help Reduce the Mortality Rate of Critical Patients
Dr. Wei-Cheng Chen, V.S., Division of Pulmonary and Critical Care Medicine, CMUH explained that ARDS is a kind of diffuse pulmonary alveoli injury with fast progression that is accompanied with severe hypoxemia. It is a cross-specialty syndrome in critical care medicine, whose common causes may include all kinds of pneumonia, sepsis, lung contusion, pancreatitis, etc. Patients may be admitted to the ICU due to respiratory failure and multiple organ failure. Such conditions consume considerable medical manpower, and resources, and interprofessional cooperation. After the worldwide COVID-19 pandemic, most people suffered from mild disease. However, more than 6.68 million people had died because of the pandemic by this January, and ARDS is common for those critical COVID-19 patients.
Dr. Wei-Cheng Chen further explained that ARDS is a pretty troublesome complication. As shown in the literature, the mortality rate of ARDS could be up to 80% in elderly and septic patients, even though respiratory treatment technology is significantly improved in modern medicine. Most ARDS patients need endotracheal intubation to survive and also need a timely diagnosis with a series of treatments to improve the prognosis. “Lung Protective Ventilation (LPV)” is currently the best treatment strategy with a strong evidence base. Dr. Wei-Cheng Chen stated that the unsatisfactory implementation rate is raised by many domestic and international studies because the timing of the cross specialty care team intervention cannot be properly and accurately integrated. At China Medical University Hospital, the pulmonologists and critical care specialist have invited their colleagues to form the cross-specialty “ARDS team.” In addition to nurse specialists, RT team, perfusionists, pharmacists, and nutritionists, the cardiovascular surgeon and physicians from emergency medicine were also invited; the most valuable part was inviting the information experts of the smart medicine system into the team as well. Through the Power business intelligence (BI) developed by Microsoft and introduced in 2021, the medical information and data of the ARDS patients were all visualized and integrated to be calculated by the system to provide real-time big data to support the medical team. As a result, the medical team can provide individualized therapeutic strategies for ARDS patients based on the data. Under such a treatment model, most critical ARDS patients can successfully recover due to the conditions reversed by proper assessment and precise treatment implementation.
Outstanding Achievement of CMUH ARDS Team Published by Top International Medical Journal <Critical Care>
CMUH “ARDS team” applied the smart medicine system improved interface to help the cross-specialty team have a real-time visualized Dashboard to obtain universal control of the patient’s medical data to cure the rapidly changing ARDS. Such excellent clinical care performance was highly recognized by the top international medical journal for emergency and critical care, “Critical care,” and the related achievements were published in the journal in August 2022 with an article entitled “Using real‑time visualization system for data driven decision support to achieve lung protective strategy: a retrospective observational study.”
The outstanding achievement of CMUH’s cross-specialty “ARDS team” on the critical care medicine was highly recognized by international emergency and critical care experts. The clinical research was published in an international journal with high Impact Factor of 19.3. Furthermore, Dr. Wei-Cheng Chen earned many domestic and international recognitions, including the best presenter and young investigator award at TSCCM/TSECCM/JSICM Joint Congress, TSECCM quality award, cross territory holistic health care best oral presentation award, first place of Taiwan Al Academy industrialization innovation competition, educational innovation award, and more.
Dr. Chieh-Lung Chen, Division of Pulmonary and Critical Care Medicine, CMUH, mentioned that, based on the APACHE II score, the level of critical conditions of ICU patients can be reflected, with a score over 20 belonging to the high risk group. After assessment, Ms. Chang had a score of 30 with a predicted mortality rate of 70%. Under the aggressive care of the ARDS team, Ms. Chang was given antibiotics and antivirals, in addition to the LPV strategy, so her critical condition improved with 15 days of ECMO support. On the 23rd day, the endotracheal tube was successfully removed, and Ms. Chang stabilized and was discharged after 35 days of hospitalization. Dr. How-Yang Tseng, who collaborated with the Information Technology Office to create the “ARDS real-time monitoring dashboard,” added that Power BI consolidates all the medical data from different sources under the system and reflects them in the real-time monitoring dashboard to show the conditions and data trends of each patient. For example, doctors could monitor all the patients’ condition through the unit distribution graph presenting with the ratio of ventilator, vasopressor, and continuous dialysis usage. According to the PF ratio, the related information would be ranked in a descending sequence to accelerate patient screening for identifying the target patients. Furthermore, it may help medical staff to quickly control the condition changes of patients so the LPV treatment strategy can be implemented earlier to elevate the cure rate.
Attachments
- Figure 1: 46-year-old Ms. Chang was suffering from ARDS due to a COVID-19 infection; she was admitted to the ICU with endotracheal intubation and ECMO applied for emergency. The team applied the smart medicine system to care for Ms. Chang and successfully control her condition to discharge her after removing the endotracheal tube. From left to right, the chest X-ray series shows the bilateral pulmonary infiltration quickly progressing but gradually subsiding after treatment.
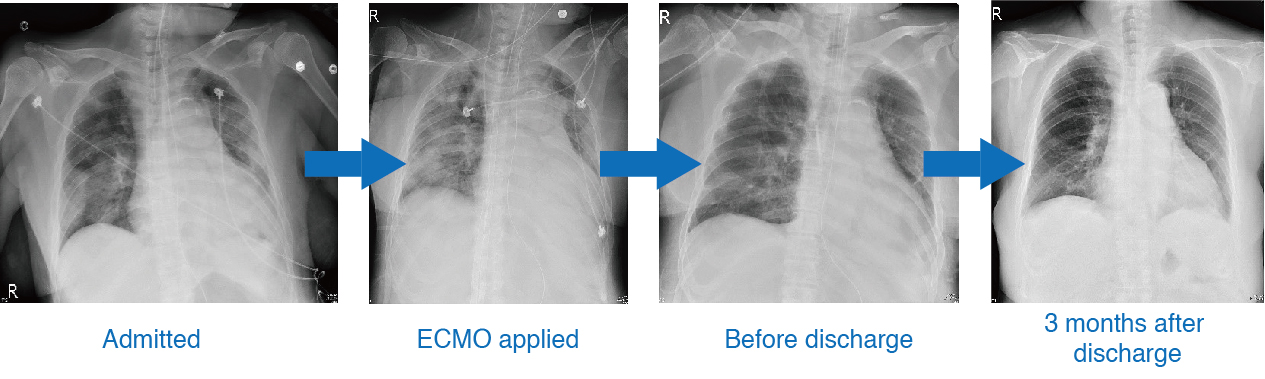
Figure 2~4: “Smart medicine system: ARDS real-time monitoring dashboard” applied to consolidate the patients’ conditions in the unit and quickly screen for ARDS patients and related information.
- Figure 2: ICU smart medicine system can timely monitor the safety of the patient universally.

- Figure 3: “Smart medicine system: ARDS real-time monitoring dashboard” ensured Ms. Chang’s “LPV,” the green zone
linemeant the safety range of the lung volume during the acute phase for patient’s lung protection.
- Figure 4: “Smart medicine system: ARDS real-time monitoring dashboard” can help consolidate the overall and individual patient severity and mortality rate in ICU to raise awareness.
- Figure 5: 46-year-old of Ms. Chang got COVID-19 and developed critical “ARDS.” CMUH put together a cross-specialty “ARDS team” with the ECMO applied. The “Smart medicine system: ARDS real-time monitoring dashboard” helped to interpret the disease conditions and reverse the critical status of Ms. Chang so she could recover and be discharged after 35 days of hospitalization.
(From left to right of the front row: Dr. Ji-Gong Deng, V.S, Division of Pulmonary and Critical Care Medicine, Dr. Wei-Cheng Chen, V.S., Division of Pulmonary and Critical Care Medicine, Ms. Chang’s older sister, Patient 46-year-old Ms. Chang, Dr. I-Ru Chen, Director of Division of Renal Transplantation)
(From left to right of the back row: Dr. How-Yang Tseng, V.S, Division of Pulmonary and Critical Care Medicine, Dr. Mao-Wang Ho, Director of Division of Infectious Disease, Dr. Chieh-Lung Chen, V.S, Division of Pulmonary and Critical Care Medicine)

- Figure 6: The CMUH ARDS team integrated the smart medicine system with physicians from different specialties, nurse specialists, the RT team, IT experts, pharmacists, and nutritionists to save the ARDS patients with all of their efforts. Patients can recover and be successfully discharged, going from the critical status that the original system predicted of 70% to just 40%.
- Figure 7: CMUH smart medicine can improve clinical care via integrated visualized information and assist cross-specialty teamwork and was thus featured in the top international medical journal <Critical care> to be shared with peers.




