News and Award
About CMUH
Operating Surgery “without Open Heart Surgery” Ventricular Septal Defect (VSD) without Surgical Procedures
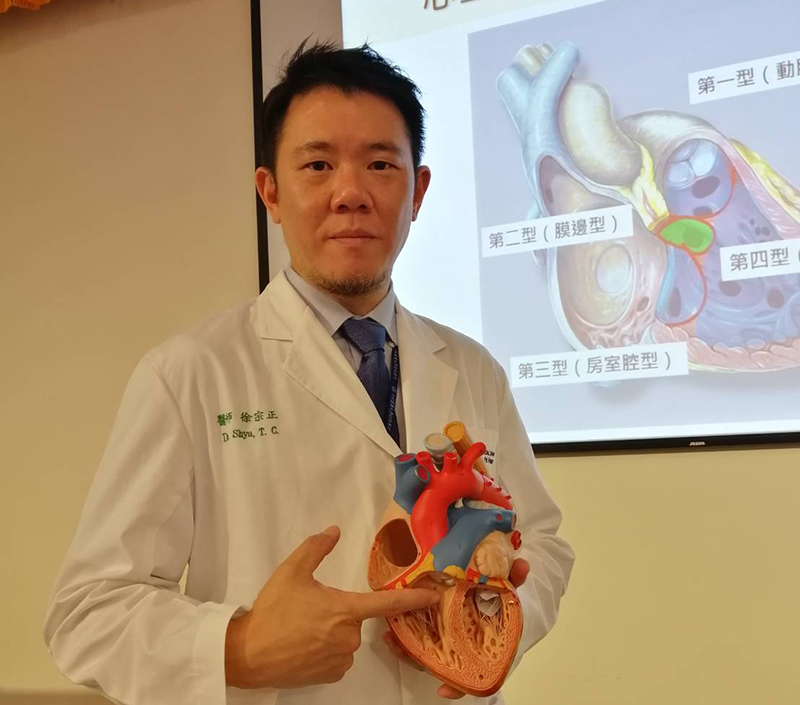
Department of Cardiac Catheterization in Children, Director Tsung-Cheng Shyu
Three-year-old little girl, Yeh, was diagnosed with a large ventricular septal defect right after birth. She suffered from symptoms such as respiratory asthma, fast heartbeat, hepatomegaly, night sweats, and slow weight and growth (her weight has fallen under 3 percentile) due to the complications with heart failure since infancy and needs to take heart failure medicine over a long period of time. However medical administration still results in the burden on the heart of Yeh and hence the hospital discussed with the family for treatment alternatives: one is to receive the traditional operating surgery and the other one is the surgery to close the ventricular septal defect via cardiac catheterization. Because of the risks of general anesthesia associated with traditional operating surgery, long hospitalization time, post-surgery scars on the chest, and other issues, the family chose cardiac catheterization to close the ventricular septal defect successfully. Yeh has eventually recovered from subsequent follow-up and is now 4 years old. She can exercise normally without symptoms while her weight has exceeded the 50th percentile.
Director Tsung-Cheng Shyu of the Department of Cardiac Catheterization in Children, China Medical University Hospital explained that a normal heart comes with the left and right ventricles, and the ventricular septum positioned in the middle for separation. Ventricular septal defect refers to a hole in the ventricular septum. Ventricular septal defect is the most common congenital heart disease, accounting for 33% of all congenital heart diseases. Approximately one in every 300 live births is one baby with ventricular septal defect. Ventricular septal defect can be divided into four types according to the position of defect in ventricular septum, and among which, Type II (Perimembranous) is the most common type, accounting for about 70%. Clinically, the symptoms shown in patients are related to the size of ventricular septal defect. Small defect may not cause any symptoms throughout the patients’ life and only could be heard of abnormal heart sounds during auscultation. However, patients with larger defect will have massive blood shunt that result in heart failure and patients are likely to suffer from shortness of breath, cold sweat, susceptibility of respiratory tract infection, and slow growth. In some cases, patients could suffer from infective endocarditis, recurrent pneumonia, pulmonary hypertension, and other complications.
Director Tsung-Cheng Shyu mentioned that for heart failure symptoms caused by larger ventricular septal defect, patients will usually be given medication to control the symptoms. Some defects will automatically shrink during follow-up but some will need to receive surgical procedures due to continuous heart failure. Surgical treatment can be further divided into traditional operating surgery or cardiac catheterization. Currently the National Health Insurance reimburses for the occluder in Type II (Perimembranous) and Type IV (Muscular) VSD. Nonetheless due to the different conditions in each person, whether the patients need to receive treatment, when to receive treatment, and which treatment, the size and shape of ventricular septal defect, age of patients and manifestation of clinical symptoms, are all basis of evaluation and the patients must discuss with the physician from Division of Pediatric Cardiology for the optimal treatment approach.



![[Taiwan–Malaysia Medical Innovation Forum] CMUH and UNIMAS Co-Host Major Medical Symposium to Advance Medical Technology and Precision Patient Care img](/FileUploads/News/20250714_131324.jpg?w=250&h=180&mode=crop&scale=both)