News and Award
About CMUH
Long-Term Lower Back Pain and Sudden Changes in Previously Well-Controlled Blood Sugar Levels Could be Precursors to Pancreatic Cancer
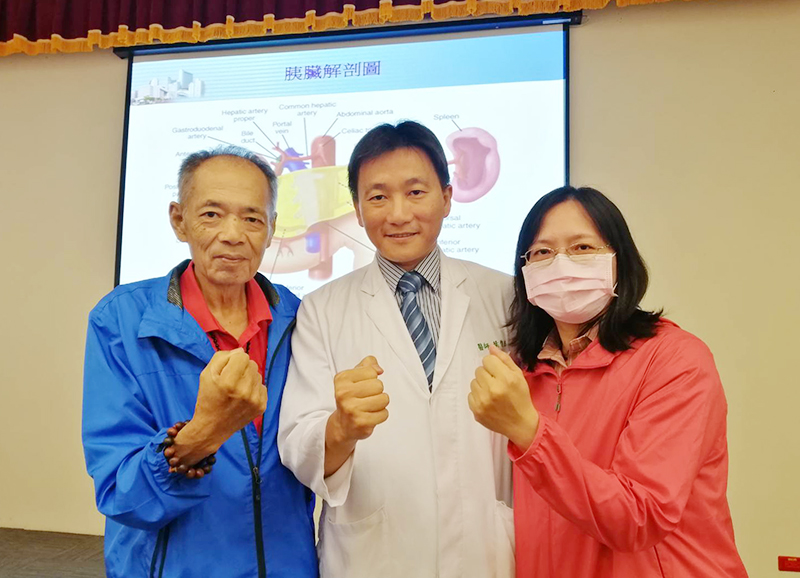
Department of Surgery Attending Physician/ Associate Professor Chun-Chieh Yeh
Pancreatic cancer is the invisible killer among all cancers mainly because it does not have early symptoms or have a reliable and effective routine follow-up and screening instrument. Once diagnosed with pancreatic cancer, patients are usually in the intermediate and advanced stages of cancer. According to statistics, only one fifth of patients have the opportunity to receive curative treatment. Moreover, pancreatic cancer is particularly susceptible to invasive metastasis and failure to diagnose early, or the slightest hesitation, can often lead to incurable metastasis.
China Medical University Hospital (CMUH) Department of Surgery – Attending Physician Chun-Chieh Yeh reported that one 41-year-old female patient suffered from unknown lower back pain for over a year and a half. In the month prior to seeking medical treatment at CMUH, her lower back pain hurt so much that she could not lie down and sleep. The patient was diagnosed with pancreatic cancer invading the peripheral nerves of her truncus coeliacus, which led to her severe lower back pain. Under the evaluation conducted by CMUH Pancreatic Cancer Therapy Team, the patient still have the opportunity to undergo curative treatment despite the difficulty with surgery. In the 2 days after visiting the outpatient clinic, the patient immediately received curative surgery in the pancreatic tail and was discharged from the hospital 1 week later. The patient was able to resolve lower back pain problem after surgery and could finally lie down to sleep. Subsequently, the patient received 6 months of adjuvant chemotherapy and has not had recurrent signs of cancer in the 2 years after the surgery.
Department of Surgery Physician Chun-Chieh Yeh also described another case, where a 67-year-old male patient was examined for poor blood sugar level control due to unknown reasons and was suspected of having a tumor at the top of the pancreas. Nonetheless, the pre-surgical pathological biopsy did not show cancer and surgical treatment was delayed for 2 months. Two sites of peritoneal carcinomatosis were observed from the surgery, which belonged to terminal pancreatic cancer that traditionally could not undergo curative surgery treatment. Fortunately, under the cooperation by CMUH cancer therapy teams, the patient first underwent five months of new adjuvant chemotherapy before receiving a second surgery. After the patient was verified for not having any metastatic lesions, the patient then underwent curative excision of the top of the pancreas. As of now, the patient does not have any signs of cancer recurrence in the 6 months after surgery and the previous diabetes was cured without having to take any antidiabetic medications. The experience of these two patients reveal the difficulty in diagnosing pancreatic cancer and the importance of having professional multidisciplinary teams (MDT) that carry the attention and enthusiasm for curing patients with pancreatic cancer.
Currently, the concept of pancreatic cancer treatment is changing substantially. Since pancreatic cancer is difficult to diagnose and can easily become metastatic, the National Comprehensive Cancer Network (NCCN) guideline currently suggests that physicians encourage patients to receive surgery if there is a likelihood for curative surgery in cases where patients are highly suspected of pancreatic cancer, even if there is no pre-surgically validated pathological diagnosis. Curing pancreatic cancer is similar to firefighting, requiring acute treatment since the slightest delay can cause patients to miss out on the opportunity for a cure. Pancreatic cancer is slowly becoming detached from the bad reputation of an incurable disease. With the multi-collaborative treatment from professional cancer teams, including surgery, chemotherapy, radiation therapy, and even cell therapy in the near future, patients should not give up so easily, even when there is a possibility of terminal pancreatic cancer. Physician Chun-Chieh Yeh also called for patients to pay attention to any possible precursors to pancreatic cancer, such as having lower back pain or upper abdominal pain for unknown reasons over a long period of time, sudden poor control of previously well-controlled diabetes for unknown reasons, yellow skin or eyes, grey-white bowel movements, brown urine, poor appetite, and loss of weight.



![[Taiwan–Malaysia Medical Innovation Forum] CMUH and UNIMAS Co-Host Major Medical Symposium to Advance Medical Technology and Precision Patient Care img](/FileUploads/News/20250714_131324.jpg?w=250&h=180&mode=crop&scale=both)