What is rheumatoid arthritis?
Rheumatoid arthritis (RA) is a chronic and progressive inflammatory joint disease that can affect all of peripheral joints. Rheumatoid arthritis can occur at any age, but is most common in middle-aged women.
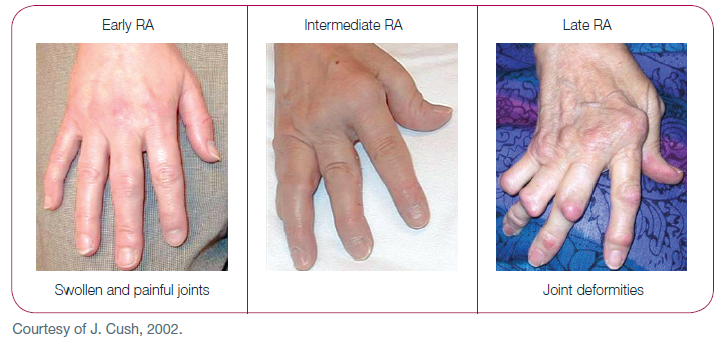
RA is characterized by chronic inflammation of articular synovium in the extremities. The early symptoms are mainly joint swelling and pain, and most of them are symmetrical. As the disease progresses, cartilage and bone are gradually eroded, resulting in joint deformation and loss of function.
The immunopathogenesis of RA is mainly an autoimmune reaction, which produces autoantibodies and inflammatory mediators (such as cytokines) that destroy articular structures and even internal organs. In addition to attacking joints, these antibodies or inflammatory mediators may also affect other organs, such as the liver, spleen, lungs, nervous system, lymphatic system, etc.
- By taking blood samples for rheumatoid factor (RF) and anti-cyclic citrullinated peptide antibodies (Anti-CCP Abs) or anti-citrullinated peptide antibodies (ACPAs). Hence, RA patients can be stratified into two groups: sero-negative and sero-positive. These autoantibodies not only aid to make diagnosis, it can also help doctors choose the most suitable treatment for you.
Clinical manifestations of rheumatoid arthritis?
- Early manifestations
About 10 percent of patients present with acute polyarthritis, joint pain, often accompanied by systemic symptoms, including fever, swollen lymph glands, or an enlarged spleen. About one-third of patients begin with monoarthritis or oligoarthritis, and about two-thirds of patients begin with only some atypical discomfort, such as fatigue, general weakness, and dull pain in bones and muscles, before developing persisted synovitis.
- Articular manifestations
The most common joint symptom of rheumatoid arthritis is pain, which is aggravated during movement. Joint stiffness occurs after prolonged inactivity (such as morning stiffness). For example, when you wake up in the morning, synovitis will cause joint swelling, tenderness, limitation of joint movement, typically involving the PIP and MCP joints of both hands, and wrist joints. Early elbow involvement can lead to limited extension and flexion, while knee involvement can lead to chronic joint effusion or a Baker's cyst. Feet and ankles will also be affected, and vertebrae can easily lead to the cervical vertebrae. In serious cases, it will cause half dislocation of the 1st and 2nd segments of the cervical vertebrae and compress the spinal nerves. After a long period of inflammation, rheumatoid arthritis can cause specific joint deformations.
- Extraarticular involvement
Patients who have a high titers of rheumatoid factor of ACPA are prone to have extraarticular involvement, including:
- Rheumatoid nodule: this may be due to local vasculitis. It mainly occurs around the joint and the extensor surface. Pathologically, it can be seen that necrosis tissue is in the central area, phagocytes are in the periphery, and connective tissue is in the outermost layer. About 20-30% of untreated and active RA patients will have this disease.
- Eyes: dry eyes and scleritis.
- Vasculitis: including finger arteritis, peripheral neuropathy, epidermal ulcer, palpable purpura, pericarditis and visceral arteritis. Pathologically, it can be seen that it is panarteritis, with monocyte as well as neutrophils infiltration in all layers of vascular wall, and endometrial hyperplasia can lead to thrombus.
- Pulmonary involvement: pulmonary hypertension, bronchiolitis, pulmonary nodules, pulmonary fibrosis, pleurisy, and interstitial lung disease (ILD).
- Kidney disease: RA rarely invades the kidney, most of which is caused by indirect causes, such as amyloidosis and side effects of medication, which can be fatal.
- Heart: pericarditis, myocarditis, endocarditis and so on, mostly related to cardiovascular inflammation or granulation tissue hyperplasia. In addition, the risk of cardiovascular or cerebrovascular disease is significantly increased, as is the risk of diabetes.
How to make diagnose of rheumatoid arthritis?
RA is mainly a clinical diagnosis. Physicians generally use the recommendations of the American College of Rheumatology (1987) as the criteria to reach the diagnosis if patients meet the following four or more conditions:
- Wake up in the morning with stiff joints and a feeling of stiffness lasts for more than an hour.
- Three or more joints are inflamed and last for more than 6 weeks.
- The finger joint is inflamed and lasts for more than 6 weeks.
- Symmetrical arthritis lasts for more than 6 weeks.
- Subcutaneous nodules (rheumatoid nodules) can be felt in specific parts of the body.
- Serum rheumatoid factor (an autoantibody) is positive.
- X-ray examination of the joint showed a pathological changes.
In the past, it took six weeks to diagnose rheumatoid arthritis, and the skeleton needed obvious damage, so some patients are often diagnosed too late. Therefore, in 2010, the European and American rheumatologists jointly published a new version of the diagnostic criteria, in order to diagnose high-risk patients early and treat them early.
- Rheumatoid arthritis classification criteria: 2010 ACR/EULAR collaborative initiative. [Ann Rheum Dis. 2010;9:1580-88].
|
Diagnostic items
|
Score
|
|
A. Joint involvement
|
|
|
1 large joint
|
0
|
|
2-10 large joints
|
1
|
|
1-3 small joints (whether or not the large joint is involved)
|
2
|
|
4-10 small joints (whether or not the large joint is involved)
|
3
|
|
>10 joints (at least one small joint)
|
5
|
|
B. Serological indicators (at least one needs to be tested)
|
|
|
RF negative and ACPA negative
|
0
|
|
RF weak positive and ACPA weak positive
|
2
|
|
RF strong positive and ACPA strong positive
|
3
|
|
C. Acute inflammatory index (at least one needs to be tested)
|
|
|
CRP normal and ESR normal
|
0
|
|
CRP abnormal and ESR abnormal
|
1
|
|
D. Duration of symptoms
|
|
|
< 6 weeks
|
0
|
|
≥ 6 weeks
|
1
|
What is the course of rheumatoid arthritis?
The course of rheumatoid arthritis usually alternates between "active" and "remission." The rate of progression varies among RA patients. The initial reaction may be inflammation of the synovium in the joint. Once the opportunity for treatment is delayed, the joint will eventually be destructed and become to be deformed, and then loss of joint function.
Before diagnosis of RA
- Little impact on daily work
- Obvious coexisting diseases
- Possible family history
Year 1
- Start having an impact on work
- Relevant medical expenses are not high
Year 2-Year 5
- Often unable to work and have to ask for leave
- Starting to have sustained moderate medical spending
After Year 5
- Incapacitation is more serious, unable to work
- Huge medical costs are required, such as joint replacement surgery

