Introduction
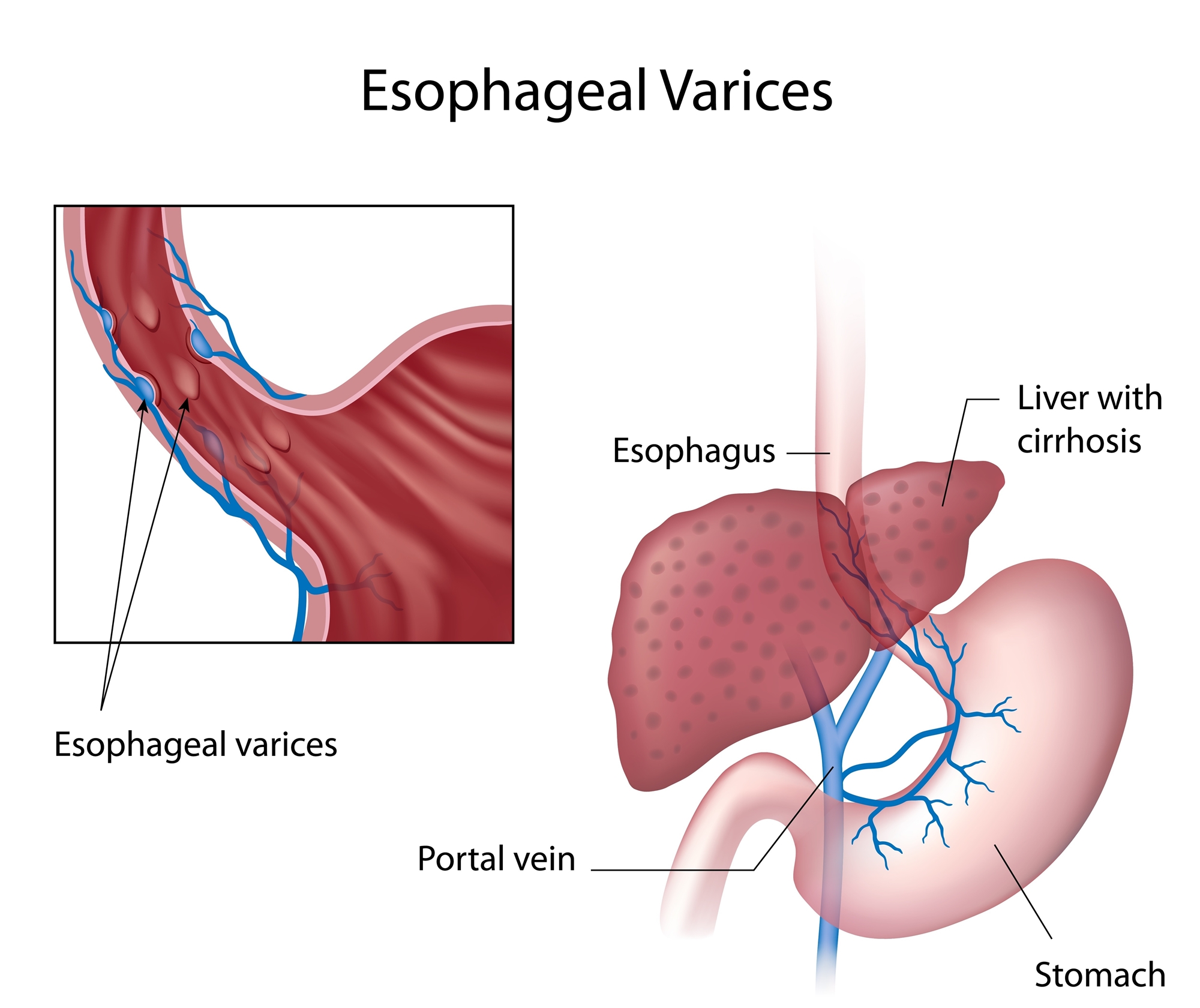
Liver cirrhosis can cause portal hypertension, unusually elevated in portal-venous pressure, may result in several complications. Esophageal variceal bleeding is one of the severe complications.
Definition and Pathogenesis
Liver cirrhosis is the most common cause of esophageal variceal bleeding. Normal portal pressure is approximately 5-10mmHg. When portal pressure is more than 12mmHg, it can result in collateral circulation, esophageal varices, and hyperactivity of systemic circulation. It commonly results from increased resistance to portal blood flow.
Clinical features and Diagnosis
Cirrhotic patients with esophageal varices do not always have rupture or hemorrhagic varices. Once there is bleeding, it usually presents with hematemesis, melena, tarry stool or even bloody stool. Additionally, there could be associated signs ranging from mild postural tachycardia and unstable blood pressure to profound shock, depending on the extent of blood loss and degree of hypovolemia.
Diagnosis is essential according to the finding of endoscopic examination and whether there is a cirrhosis history. Endoscopy is the best approach to evaluate upper gastrointestinal hemorrhage in patients with known or suspected portal hypertension.
In patients with known liver disease, the development of portal hypertension is usually revealed by the appearance of splenomegaly, ascites, hepatic encephalopathy, and/or esophageal varices. Commonly, the finding of any of these features should prompt evaluation for possible portal hypertension and liver disease.
Treatment
Treatment includes non-surgical and surgical intervention.
- non-surgical intervention:
- vasoconstrictors: like terlipressin and somatostatin. Acute treatment with these medications may help control acute variceal bleeding.
- balloon tamponade: control bleeding by compress the gastric or esophageal bleeder.
- endoscopic variceal sclerosis (sclerotherapy): sclerosant is injected into esophageal varices to achieve efficacy of reducing or stop bleeding.
- endoscopic variceal ligation (EVL): after identifying the bleeding site of esophageal varices by endoscopy, ligation is performed. Because EVL has less recurrent rate of vertical bleeding with fewer local complications, it requires fewer treatment sessions to achieve variceal eradication as compared to sclerotherapy. EVL becomes the major therapeutic method now.
- surgical intervention:
- transjugular intrahepatic portosystemic shunt (TIPS): relieving portal hypertension can be accomplished without surgery through the percutaneous stent placement of a portal-systemic shunt.
- Directly surgical eradication of esophageal or gastric varices.
Notices
- pay attention to hematemesis and melena.
- avoid too hot or too cold food. Additionally, rigid medication should be powdered to reduce the chance rupture of esophageal variceal rupture.
- adequate exercise and enough rest and sleep.
- avoid strong cough, lifting heavy things, and hard defecation.
- call for help if there is syncope, thirsty, tachycardia or dyspnea.
- regular endoscopic evaluation and intervention if needed.

