What is peptic ulcer disease?
Peptic ulcer disease refers to painful scores or tensions in the lining of the stomach or first part of duodenum. It is typically caused by an acid resistant bacterium called Helicobacter pylori (H. pylori).
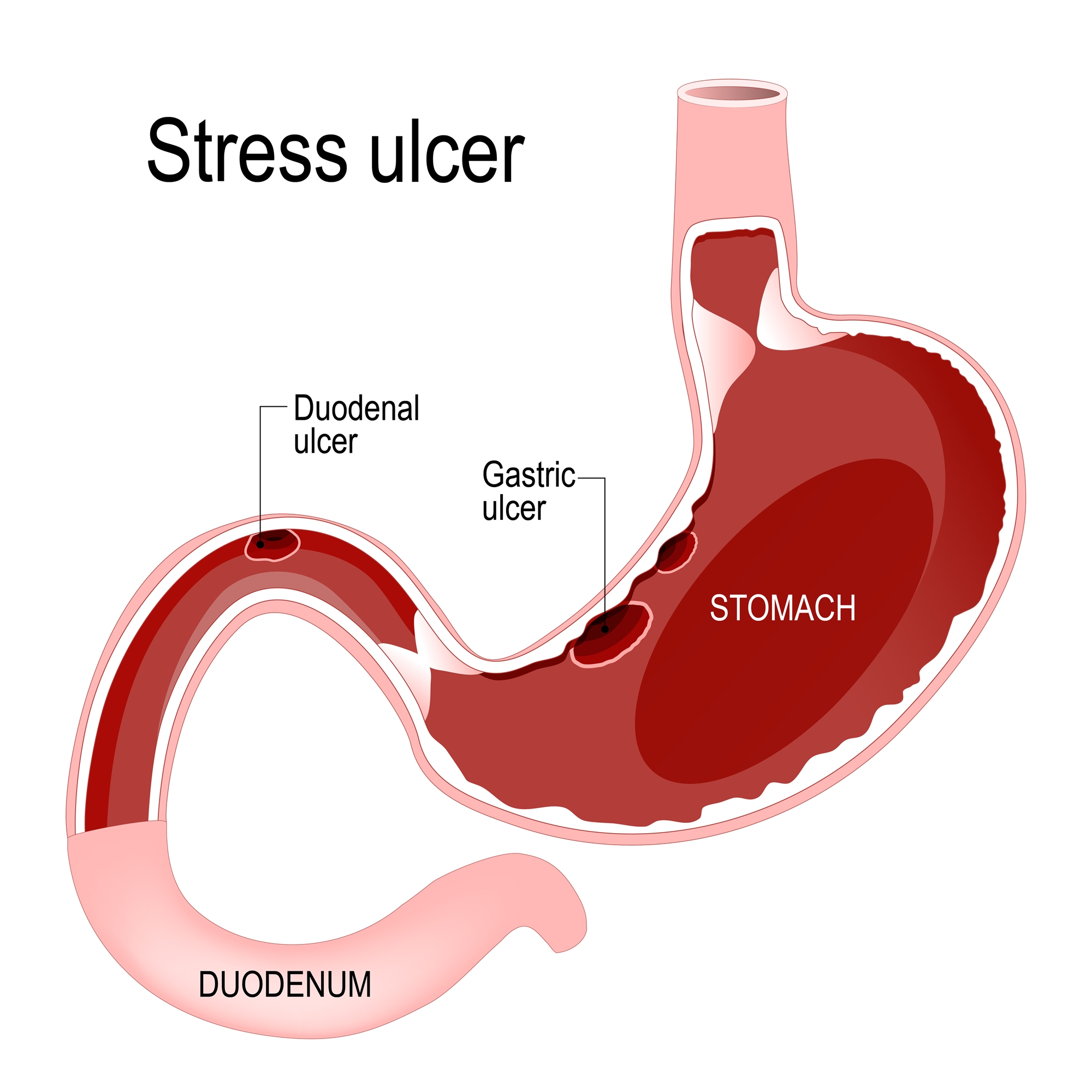
Peptic ulcers occur in the stomach and mostly in the duodenum.
- Duodenal ulcer: mostly occurs in proximal portion of duodenum which is close to pylorus. Patients feel painful in hunger and feel better after meals.
- Gastric ulcer: mostly occurs in lesser curvature side of the stomach near the pylorus. The patients usually have pains after meals. 4% of the patients are likely to have stomach cancer.
What causes peptic ulcer disease?
- Medications: frequent or longtime use of NSAID
- Stress: emotional, nervous, or stress problems.
- Inheritance tendency
- Diet: spicy food, overeating, irregular meals
- Excess smoking, alcohol, and coffee.
- Helicobacter pylori infection
Diagnosis
- Clinical symptoms, esophagogastroduodenoscopy, or upper G-I barium X-ray study.
- Symptoms: pain, bloating, vomiting, tarry stools.
Treatment for peptic ulcers
Antacids, H2- blocker such as Zantac, Tagamet, or PPI such as Losec, Takepron, Nexium, and Pariet. If you have H. pylori infection, HP eradication with antibiotics is often used for 1 to 2 weeks.
Treatment for bleeding complications:
- Intravenous acid-reducing agents: e.g., Zantac and Losec.
- Endoscopic hemostasis: after esophago-gastroduodenoscopy, the patient cannot have meals until further instructions from doctors.
- Surgery: you will only need surgery if the bleeding fails to stop, after medical and endogastric treatment or you may have complications such as perforation or pyloric stenosis.
Foods recommended for the peptic ulcer diet
Bleeding ulcers
- Stage 1: Absolutely no diet is recommended from bleeding till 2-3 days after bleeding stops. Please follow the doctor’s instruction for milk or liquid diet at room temperature.
- Stage 2: Soft food diet is recommended 2-3 days after bleeding stops to recovery stage.
- Stage 3: Regular diet is recommended during recovery unless discomfort is experienced. Keep regular diet during recovery both for bleeding or non-bleeding ulcer patients.
Notes on diet for peptic ulcer patients
- Eat a fixed quantity at fixed times
- Eat slowly and chew your food well. Remain relaxed during meals, as well as rest a few minutes before starting to work.
- Eat a soft, nutritious, easy-to-digest diet.
- Eat each meal including protein such as milk, fish, bean products, and lean meat. Avoid eating starch only.
- Eat a diet rich in vitamin C and iron.
- Items most frequently associated with gastric discomfort, for example, sweet food or food which causes bloating and gas. These should be eliminated from diet unless specifically allowed by the physician and/or dietitian. Additional adjustments may be made according to individual tolerances.
- Steam, boil, stew, or mash your foods rather than baking, grilling, or frying.
- Avoid high-fiber vegetables (e.g., tough stem or leaf), high-fiber/acidity fruits (e.g., pineapple or guava), and nuts (e.g., cashews or walnut)
- Avoid hot-spicy seasoning (chili, mustard) and drinks (tea, coffee, or alcohol)
- For patients with acute gastritis, stop meals for 1-2 days; but some water is allowed. Liquid diet is recommended afterwards. Low fat is recommended since fat would decrease gastric juice secretion.
Daily Care
- Have a regular life and avoid staying up.
- Avoid stress and emotional tension.
- Keep warm when the temperature drops.
- No smoking and no alcohol
- Bleeding symptoms: abdominal pain, nausea, fast breathing, pallor, hematemesis, and black stools.
- Follow doctor’s instruction for taking medications.
- Regular follow-up and treatment

